This post is also available in:
 Español (Spanish)
Español (Spanish)
By: Vilmar Trinta Negrón
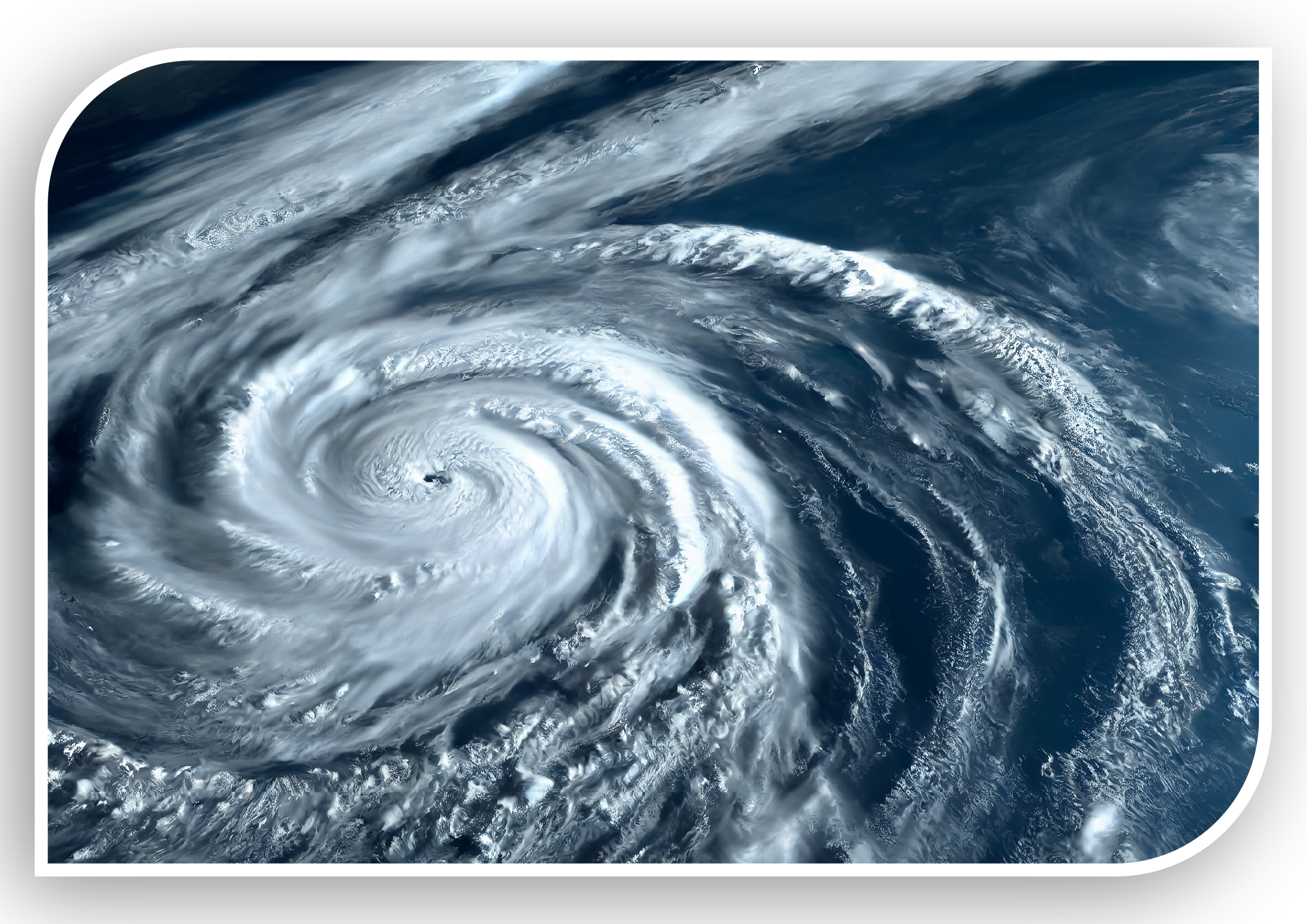 ▶ In Puerto Rico, hurricane season extends from June 1 to November 30, with the peak occurring between August and October. This period demands not only technical preparedness from healthcare providers, but also leadership, coordination, and a strong commitment to the resilience of the services they deliver. Preparation is not merely advisable—it is a legal requirement and a professional obligation to ensure patient safety, operational stability of healthcare facilities, and an efficient emergency response.
▶ In Puerto Rico, hurricane season extends from June 1 to November 30, with the peak occurring between August and October. This period demands not only technical preparedness from healthcare providers, but also leadership, coordination, and a strong commitment to the resilience of the services they deliver. Preparation is not merely advisable—it is a legal requirement and a professional obligation to ensure patient safety, operational stability of healthcare facilities, and an efficient emergency response.
The aftermath of hurricanes such as María and Fiona demonstrated that proper planning can mean the difference between uninterrupted care and a humanitarian crisis. Disruption of critical services such as electricity, water, or communications can jeopardize patients with chronic conditions who rely on oxygen, intravenous therapies, or dialysis. Additionally, many healthcare centers face logistical challenges if they lack emergency response protocols.
Emergency preparedness within Puerto Rico’s healthcare system is supported by existing legislation and operational plans established by health authorities. These plans must include specific protocols to ensure continued operations during the loss of essential services such as electricity, water, or fuel, clearly defined staff roles, and adjustments to patient flow during emergencies.
Moreover, the Puerto Rico Department of Health and the Puerto Rico National Guard (PRNG) have strengthened their collaboration to foster an effective interagency response to weather events. Their recommendations include coordination among hospitals, clinics, and municipalities; shared protocols for generator use; active monitoring of vulnerable patients; and establishing communication channels for joint decision-making during severe weather events.
Weather emergencies not only threaten physical infrastructure, but also staff availability, access to medication, and the functioning of clinical and administrative systems.
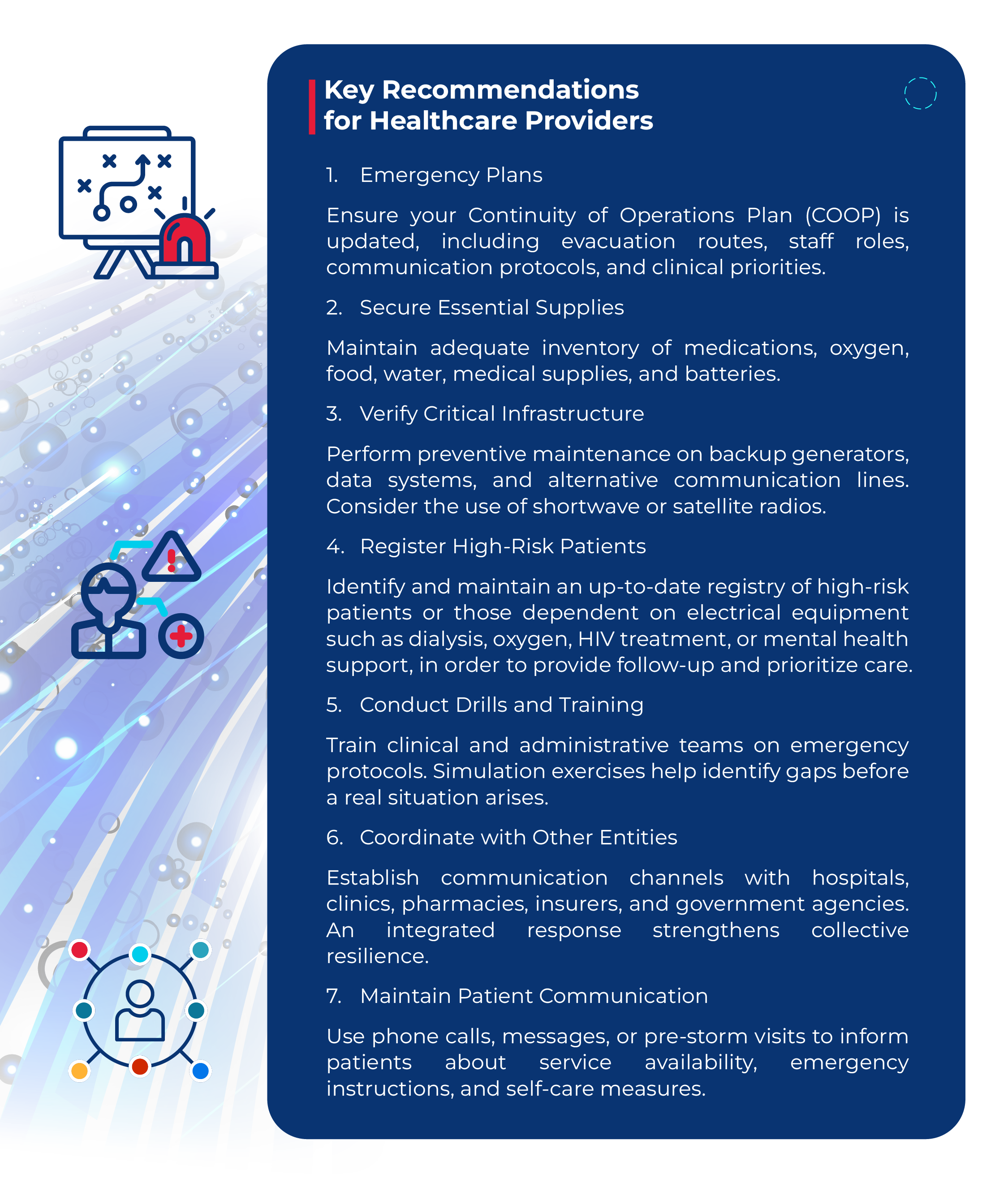
Telemedicine has emerged as a key tool for maintaining access to medical services during emergencies. Although hurricanes may disrupt communications, having redundant connectivity systems—such as satellite networks—allows for continued remote patient care.
Additionally, cloud-based electronic health records enable healthcare professionals to access vital information even when physical facilities are compromised.
The resilience of the healthcare system does not rely solely on medical institutions. Communities play a crucial role. Trained community health promoters, mobile medical brigades, and community leaders can provide first aid, identify urgent needs, and serve as liaisons to formal healthcare services.
In rural or hard-to-reach areas, it is essential to establish temporary health centers or coordinate with churches, schools, and community centers to provide basic services. This decentralized network can reduce hospital overcrowding and ensure immediate care.
 Ensuring the continuity of healthcare services during hurricane season in Puerto Rico is a complex, yet achievable challenge. Preparation is not only an institutional responsibility but also an act of commitment to the health and lives of patients. Every provider plays a vital role in community preparedness to face hurricane season. The better the preparation, the greater the capacity for response and recovery.
Ensuring the continuity of healthcare services during hurricane season in Puerto Rico is a complex, yet achievable challenge. Preparation is not only an institutional responsibility but also an act of commitment to the health and lives of patients. Every provider plays a vital role in community preparedness to face hurricane season. The better the preparation, the greater the capacity for response and recovery.
This post is also available in:
 Español (Spanish)
Español (Spanish)