This post is also available in:
 Español (Spanish)
Español (Spanish)
Redacted by Vilmar Trinta | Interviewed Lilybeth Rivera García, Coding and Premium Management Director at Provider Network Solutions of Puerto Rico (Provider PR)
Behind every code sent to an insurance company lies much more than an administrative process—each diagnosis represents a patient’s medical history, the quality of care provided, and the financial stability of an organization. That’s why clinical coding is not just a technical task; it is a shared commitment among physicians, billers, and coders.
“Every year, certified coders lead intense campaigns aimed at physicians and billers to reinforce the importance of properly documenting beneficiary diagnoses in every clinical encounter,” explained Lilybeth Rivera García, Coding and Premium Management Director at Provider Network Solutions (PNS). 
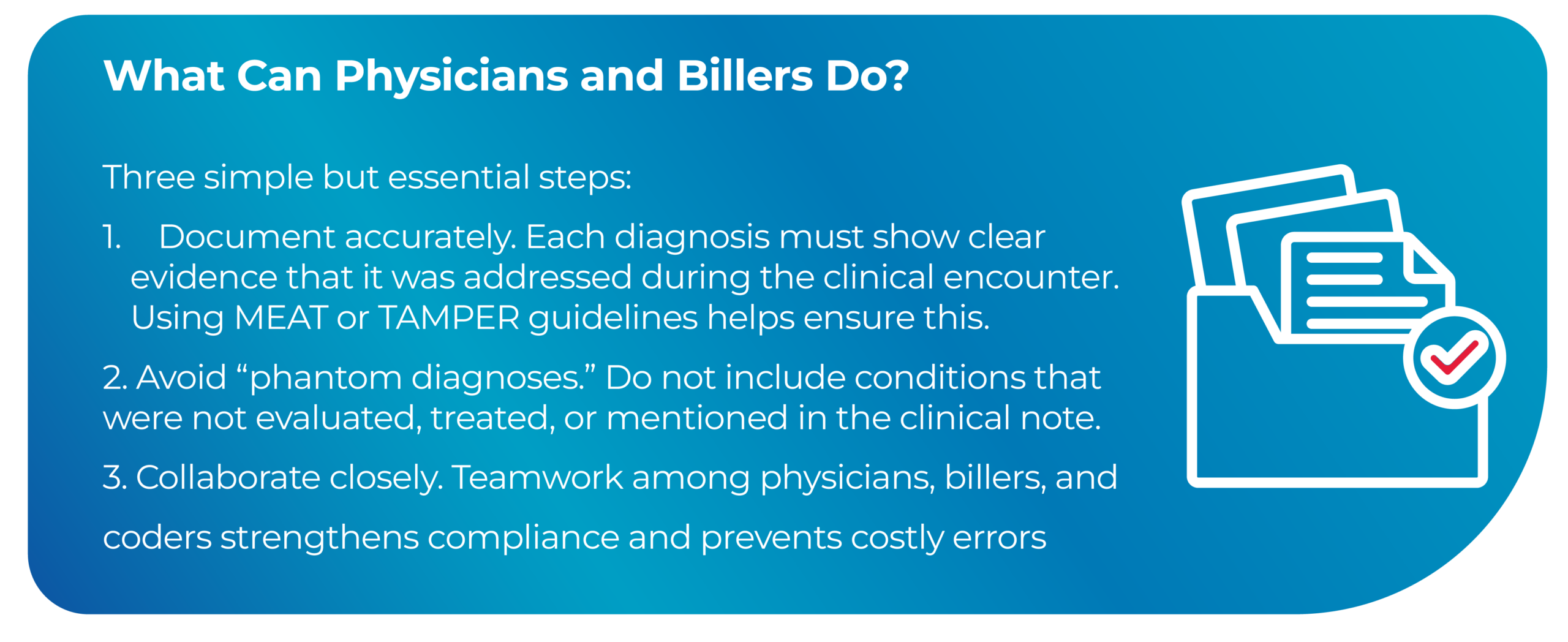
Rivera García emphasized that, for a diagnosis to be valid, it must be clearly supported in the clinical note using recognized methodologies such as MEAT (Monitored, Evaluated, Addressed, Treated) or TAMPER (Treatment, Assessment, Monitoring, Plan, Evaluation, Referral).
“If a diagnosis is not documented under these criteria, it will be considered invalid in an audit,” she stressed. Despite ongoing educational efforts, annual audits continue to reveal deficiencies in the documentation that supports diagnoses.
“We still find clinical notes lacking sufficient evidence or clear medical justification, which puts the validity of the diagnosis—and therefore regulatory compliance—at risk,”added Rivera García.
These compliance measures also apply to telemedicine. Therefore, it is equally important that virtual services be properly documented and coded.
“Every virtual encounter must meet the same documentation standards as an in-person visit,” Rivera García emphasized. “The fact that it is a remote consultation does not exempt the provider from describing the patient’s evaluation, plan, and follow-up. Everything must be recorded and clinically supported.”
This means that the MEAT or TAMPER criteria apply equally to teleconsultations. Accurate documentation not only ensures appropriate payment for the service but also protects the organization in the event of audits.
“Accurate coding is not optional. It is the foundation that protects the organization’s revenue, ensures the integrity of the medical record, and secures compliance with Centers for Medicare & Medicaid Services (CMS) regulations. A poorly documented diagnosis can result in financial adjustments, penalties, and even extrapolated audits that affect the entire practice,” reiterated Rivera García.
Medicare Advantage plans receive CMS payments based on their beneficiaries diagnoses through the Risk Adjustment Factor (RAF) model. Therefore, CMS conducts RADV (Risk Adjustment Data Validation) audits to verify that every diagnosis code is clinically supported.
Key Changes Starting in 2025
 In May 2025, CMS implemented new rules that led to much more rigorous RADV audits:
In May 2025, CMS implemented new rules that led to much more rigorous RADV audits:
- All eligible contracts will be audited, increasing from 60 to more than 550 plans per year.
- Errors found dating back to the 2018 payment year will be extrapolated to the entire contract population.
- The audit sample will increase to 200 records per contract.
- The CMS coding review team will expand from 40 to 2,000 reviewers by September 2025.
- Automated systems will be integrated to detect unsupported diagnoses.
“These measures challenge us to be more rigorous and consistent. Accurate coding becomes our best defense in this new regulatory environment,” said Rivera García.
At Provider Network Solutions Puerto Rico, the message is clear: compliance begins in the clinical note. Proper documentation not only protects the organization but also ensures that each patient receives appropriate recognition for their condition and care.
“Behind every code is a story of health and a shared responsibility,” concluded Rivera García. “When we document correctly, everyone wins—the patient, the provider, and the system.”
This post is also available in:
 Español (Spanish)
Español (Spanish)